Claims entry
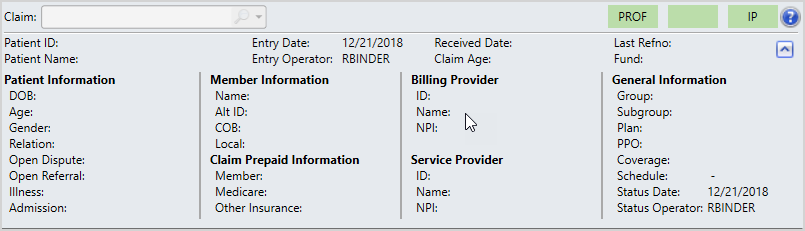
The main areas are—1) Claim snapshot, 2) viewports, 3) workspaces, 4) navigator, and 5) the star menu. These areas are described below.
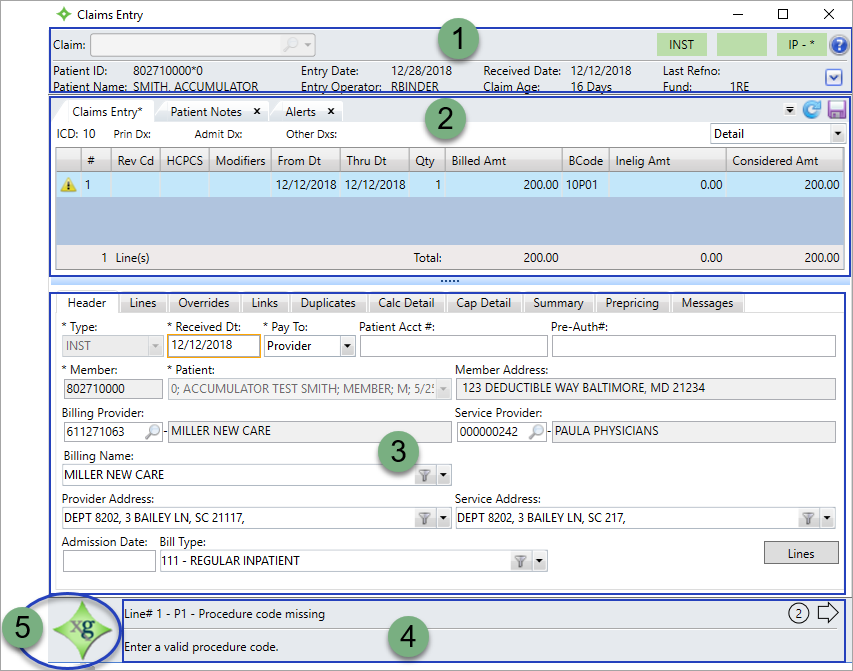
As you enter claim line information in the claim snapshot, the snapshot updates with selected information.
| Field | Description |
|---|---|
|
Claim |
Claim identification number entry/search or selection list. |
|
Green box containing the status of the claim. |

|
Green box displaying the claim type. DENT (Dental), INST (Institutional), or PROF (Professional). |
|
Green box displaying the claim number. On a claim entry, the box will be empty.
|
|
Identification number of the patient for whom the claim is being processed. |
|
|
Claim entry date. Current date if entering a claim, or the date the claim was entered if processing a claim. |
|
|
Date the office received the claim. Depending on your system settings this could be same as the Received Date.
|
|
|
The reference number of the most current claim the operator worked on. |
|
|
User who initially entered the claim. This is an automatically updated field.
|
|
|
Patient Name |
Full name of patient on the claim. |
|
The age of the claim from when it was received until now (Current Date minus the Received Date). This will only display for claims the |
|
|
Fund |
Fund associated with the member on the claim. |
|
|
Displays additional information for:
|
- Click
 to the left of the Fund field or use the
to the left of the Fund field or use the F8key to display additional claim information.
The viewports show different claim line information that you've entered or is calculated based on your system setup. Choose a viewport from the list.
Click a row in the viewport to view a different claim line. The claim line row stays highlighted, which can be a useful marker to indicate which claim line you're viewing when you switch viewports.
- Beneath the viewport area is a "splitter" that you can drag up or down to adjust the size of the viewport area.
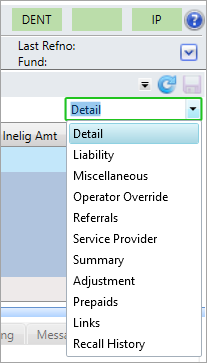
The viewports are:
ICD above the table. Institutional entry and processing viewports display the Prin Dx, Admit Dx, and Other Dxs codes if applicable. Informational viewports don’t display the codes above the table.-
Detail—Shows basic information for a claim line. For example, the from and through dates, procedure code, primary diagnosis code, and billed, ineligible, and prepaid amounts. The total billed, ineligible, and prepaid amounts for the claim show at the bottom of the table. Claim Detail viewport field descriptions
Claim Detail viewport field descriptions
Column Description #
The claim line number. If the entire claim is in Held or Audit status, then this field is blank.
Rev Cd - HIPAA
 HIPAA (Health Insurance Portability and Accountability Act of 1996) is the United States legislation that provides data privacy and security provisions for safeguarding medical information.-compliant, three-digit code consistent with the National Uniform Billing Committee.
HIPAA (Health Insurance Portability and Accountability Act of 1996) is the United States legislation that provides data privacy and security provisions for safeguarding medical information.-compliant, three-digit code consistent with the National Uniform Billing Committee. - Revenue Codes are descriptions and dollar amounts charged for hospital services provided to a patient. The revenue code tells an insurance company whether the procedure was performed in the emergency room, operating room or another department.
-
The claim schedule determines if revenue accounting is necessary for the claim line.
Note: 837I claims, may require Revenue codes.
HCPS The Healthcare Common Procedure Coding System (HCPCS) is a set of codes that standardize identification of medical services, supplies, and equipment.
- There are two sets of codes. The first, or Level I, code set is a five-digit numeric code that contains the Physicians Current Procedural Terminology (CPT) maintained by the American Medical Association.
- The second code set, or Level II is a code set for medical services not included in Level I, such as durable medical equipment, prosthetics, orthotics and supplies. These codes are alpha-numeric and begin with a single letter followed by four numbers.
Modifiers Procedure code modifiers—office or medical organization-defined codes that provide additional information concerning a particular service and can be used in the service price calculation. From Dt The start date for the service provided.
Thru Dt The end date for the service provided.
PoS Place Of Service. Numeric code describing the location where service was rendered. The codes are defined by the plan administrators but also include basys defaults.
Proc A code that identifies a specific service performed by a service provider.
Billed Amt The amount billed for the line item.
Qty The number of times the service was provided.
BCode The benefit code representing a benefit or service covered in the Summary Plan Description document (e.g. eye exam, emergency outpatient care, or an office medical visit).
Inelig Amt Considered Amt The amount considered for payment. It is calculated as follows: Billed Amount - Ineligible Amount. - HIPAA
-
Liability—Shows the patient, provider, and FSA Accounts offered and administered by employers that provide a way for employees to set aside, out of their paycheck, pretax dollars to pay for the employee’s share of insurance premiums or medical expenses not covered by the employer’s health plan. liability calculated amounts and indicates if an operator overrode one of the liability calculations.
Accounts offered and administered by employers that provide a way for employees to set aside, out of their paycheck, pretax dollars to pay for the employee’s share of insurance premiums or medical expenses not covered by the employer’s health plan. liability calculated amounts and indicates if an operator overrode one of the liability calculations.  Liability viewport field descriptions
Liability viewport field descriptions
Column Description #
The claim line number. If the entire claim is in Held or Audit status, then this field is blank.
Amount the patient owes.
Note: The amount is calculated automatically, but you can override it on the Claim Entry or Processing Overrides workspace.
Provider Liability
Amount that is the provider's responsibility.
-
For example, a provider belongs to a network and bills $90 for a procedure. The network only allows $50. If the claim is paid at 100% (no patient responsibility), then the provider is liable for the remaining $40.
Note: The amount is calculated automatically, but you can override it on the Claim Entry or Processing Overrides workspace.
PPO Discount The Preferred Provider Organization (PPO
 A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount.) discount is the amount the member saves using a network provider.
A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount.) discount is the amount the member saves using a network provider.- The PPO discount is the difference between the provider's billed amount and the PPO's allowed amount.
- If the plan doesn't use a PPO network, it will be zero.
Note: The amount is calculated automatically, but you can override it on the Claim Entry or Processing Overrides workspace.
Amount that could be FSA
 Accounts offered and administered by employers that provide a way for employees to set aside, out of their paycheck, pretax dollars to pay for the employee’s share of insurance premiums or medical expenses not covered by the employer’s health plan. eligible.
Accounts offered and administered by employers that provide a way for employees to set aside, out of their paycheck, pretax dollars to pay for the employee’s share of insurance premiums or medical expenses not covered by the employer’s health plan. eligible. - Patient Liability—Non-reimbursable Ineligible Amounts.
Note: The amount is calculated automatically, but you can override it on the Claim Entry or Processing Overrides workspace.
Overridden
A
Yesindicates an operator overrode a liability calculation (patient, provider, FSA, or PPO discount) from the Override workspace.- To see who overrode the liability calculation check the Operator Override viewport.
-
-
Miscellaneous—Shows additional information about the procedure—the laterality or specific digit affected. It also shows the revenue code if revenue accounting is used to calculate the claim line. Miscellaneous viewport field descriptions
Miscellaneous viewport field descriptions
Column Description #
The claim line number. If the entire claim is in Held or Audit status, then this field is blank.
The side of the body affected by the procedure.
L—Left side of the bodyR—Right side of the body
The toe or finger affected by the procedure.
- The possible values are 1 through 5, where the number represents a particular digit.
- HIPAA
 HIPAA (Health Insurance Portability and Accountability Act of 1996) is the United States legislation that provides data privacy and security provisions for safeguarding medical information.-compliant, three-digit code consistent with the National Uniform Billing Committee.
HIPAA (Health Insurance Portability and Accountability Act of 1996) is the United States legislation that provides data privacy and security provisions for safeguarding medical information.-compliant, three-digit code consistent with the National Uniform Billing Committee. - Revenue Codes are descriptions and dollar amounts charged for hospital services provided to a patient. The revenue code tells an insurance company whether the procedure was performed in the emergency room, operating room or another department.
-
The claim schedule determines if revenue accounting is necessary for the claim line.
Note: 837I claims, may require Revenue codes.
-
Operator Override—Shows the name of the operator that overrode the claim calculation, liability calculation, eligibility or PPO A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount. for a claim line.
A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount. for a claim line. Operator Override viewport field descriptions
Operator Override viewport field descriptions
Column Description #
The claim line number. If the entire claim is in Held or Audit status, then this field is blank.
Claim Calculation
The operator ID of the person who performed the override on the claim calculation.
Claim Calculation Date Date the claim calculation was overridden. Liability
The operator ID of the person who performed the liability calculation (patient, provider, FSA
 Accounts offered and administered by employers that provide a way for employees to set aside, out of their paycheck, pretax dollars to pay for the employee’s share of insurance premiums or medical expenses not covered by the employer’s health plan., or PPO discount) override.
Accounts offered and administered by employers that provide a way for employees to set aside, out of their paycheck, pretax dollars to pay for the employee’s share of insurance premiums or medical expenses not covered by the employer’s health plan., or PPO discount) override.- You can view the liability amounts on the Liability viewport.
Liability Date Date the claim liability calculation was overridden. The operator ID of the person who performed the override.
Eligibility date Date the claim eligibility was overridden. PPO  A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount.
A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount.
The operator ID of the person who performed the PPO override. PPO Date Date the PPO was overridden. -
Referrals—Shows the referrals for a claim line. The referral information includes the service covered by the referral, the approved number of visits or dollar amount covered by the referral, and the actual quantity used or applied. Referrals viewport field descriptions
Referrals viewport field descriptions
-
Service Provider—Shows the service provider's name, ID, and NPI A unique identifier issued by the National Plan and Provider Enumeration System (NPPES) to all health care providers who want to send or receive HIPAA transactions. The NPI is required under HIPAA legislation for all HIPAA transactions..
A unique identifier issued by the National Plan and Provider Enumeration System (NPPES) to all health care providers who want to send or receive HIPAA transactions. The NPI is required under HIPAA legislation for all HIPAA transactions.. Service Provider viewport field descriptions
Service Provider viewport field descriptions
-
Summary—Shows calculated amounts for the line item, such as the billed, considered, allowed, and covered amounts, along with any discount information. Total amounts for the claim show at the bottom of the table. Summary viewport field descriptions
Summary viewport field descriptions
Column Description #
The claim line number. If the entire claim is in Held or Audit status, then this field is blank.
The amount billed for the line item.
The amount considered for payment. It is calculated as follows: Billed Amount - Ineligible Amount.
The allowed amount. The considered amount compared to the UCR
 The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. or fee schedule amount and the lesser of the two is the amount allowed for the line item.
The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. or fee schedule amount and the lesser of the two is the amount allowed for the line item. Covered
The amount covered by providers. It is calculated as follows: (Allowed Amount - Deductibles) multiplied by (Co-Insurance %).
The amount that is covered under the plan rules. It is calculated as follows: Covered Amount - COB adjustments.
This discount amount. The discount is either:
- Net Covered Amount multiplied by Discount Percentage
OR
- a configurable discount amount ( e.g. a provider discount or a claim schedule discount)
The member share discount. This is calculated as follows: Discount (previous column) - a Discount Amount.
A code that identifies and defines the discount taken on the net covered amount.
Note: Discounts taken on billed or considered amounts are considered as ineligible amounts.
The actual benefit amount paid. It is calculated as follows: Net Covered Amount - Discount Amount.
-
Adjustment—Displays claim information that was adjusted for various reasons, including claim underpayment or overpayment, prior payments adjustments, or disputed case credits. Adjustment viewport field descriptions
Adjustment viewport field descriptions
Column Description Adj Seq Adjustment Sequence. Sequence number for the claim adjustment. Claim Ref# Reference number for the adjusted claim. Status The status of the claim. See the Claim statuses topic for descriptions.
Adjusted From Reference number of the original claim that was adjusted to a new claim.
- For example, if claim A100 is the original claim, the new claim, A102, was adjusted from A100.
Adjusted To Reference number of the new claim that was adjusted from the original claim.
- For example, if claim A102 is the new claim, the original claim, A100, is adjusted to A102.
Action Date The last date any adjustment changes were made to the claim.
Reason Code A code that identifies the adjustment reason. These codes can be site specific.
AD—admission choice errorBA—billed amount errorBC—benefit code errorBP—billing provider choice errorBQ—billed quantity errorCB—COB/prepaid entry errorCD—check damagedCL—claimant choice errorD—diagnosis errorDC—disputed case choice errorDP—duplicate claimDS—dates of service errorIL—illness choice errorPA—provider address errorPO—payment override errorPP—PPO choice/pre-priced entry errorPR—procedure errorRD—received date errorRF—referral choice errorRS—referral service choice error
Adj Operator Adjustment Operator. The operator ID of the person who made the change. Prior Pay Adj The prior payment amount for the associated claim, if applicable. Paid Amt The actual benefit amount paid. It is calculated as follows: Net Covered Amount - Discount Amount. -
Prepaids—Displays the member, Medicare, and other prepaid amounts as well as their totals.Note: Prepaid amounts apply at each line, not at the claim level. Prepaids viewport field descriptions
Prepaids viewport field descriptions
-
Recall History—Shows information related to a released claim that was recalled including the date and time, the operator that recalled the claim, and the prior release operator. Recall History viewport field descriptions
Recall History viewport field descriptions
Most claims entry workspaces allow you to enter various claim information including patient and provider demographics. The exceptions are the Cap Detail, Summary, and Duplicates workspaces which are view only and can't be updated.
The workspace tabs are:
-
Header—Enter the information that will display in the snapshot : the basic claim information such as the claim type, when it was received, the member, and billing information, etc. Once the required fields are completed, a Lines button becomes active, allowing you to access the Lines workspace. Header workspace field descriptions
Header workspace field descriptions
* indicates a required field
Field Claim Type Description Type *
All Claim type. This is a read-only field. Change the claim type
DENTINSTPROF
All Received date. The date the office received the claim.
- Enter or update the date in MM/DD/YYYY format (e.g. 01/05/2018 or 01052018).
- You can use the following date separators: (., -, /) or don't enter any separators.
- If your system is configured to tab over the date, it defaults to the current date.
Important: If you resolved a claim's pends or copied a duplicate claim's data, the Received Date might not be the original received date. Depending on your software version, you might see a
 next to the Received Date field. Hover over this icon to view the claim's original received date.
next to the Received Date field. Hover over this icon to view the claim's original received date.Pay To *
All Indicates who the payment will be made to:
Member.Provider.
Patient Acct #
All Patient account number.
Pre-Auth#
All Pre-authorization number.
Member *
All Member ID number.
Patient * All Patient associated with the claim.
Member Address All Address of the member associated with the claim. Institutional only Bill type is a 4-digit code that applies to institutional claims, where each digit identifies specific information:
- 1st digit is a leading zero and isn't used in Service.
- 2nd digit is the facility type.
- 3rd is the bill classification.
- 4th is the submission frequency.
All The tax ID number for the billing provider or organization that issued the bill for the services listed on the claim.
Hint: Enter a character or two in a provider box and then click
 to display a look-up window where you can search for the provider.
to display a look-up window where you can search for the provider.All The ID number for the provider who renders the services submitted by the billing provider.
Hint: Enter a character or two in a provider box and then click the
 icon to display a look-up window where you can search for the provider.
icon to display a look-up window where you can search for the provider.All The individual or organization that issued the bill for the services listed on the claim.
Provider Address
All The address for the billing provider or organization that issued the bill for the services listed on the claim.
Service Address All The address of the performed services listed on the claim. Admission Date Institutional only Date the patient was admitted.
- Enter or update the date in MM/DD/YYYY format (e.g. 01/05/2018 or 01052018).
- You can use the following date separators: (., -, /) or don't enter any separators.
Dental and Professional only Related Condition. Condition(s) related to the claim, such as Accident, Illness, or Work Related.
Dental and Professional only Date the illness or accident occurred.
Professional only ID number of the referring physician.
Place of Treatment (PoS) Dental only Place Of Service. Numeric code describing the location where service was rendered. The codes are defined by the plan administrators but also include basys defaults.
-
Lines—The Lines workspace is tailored to the specific professional, institutional, and dental forms and contains the necessary values for each (Professional CMS 1500 Claim Form, Institutional CMS 1450/UB-04 Form, and Dental – ADA Form). See International Classification of Diseases (ICD) codes that describe diagnoses. These codes are used for diagnostic, billing, and reporting purposes. .Hint: In an empty code field, use the keyboard shortcutCtrl+Lto look up or search for the code. Use the keyboard shortcutCtrl+Dto display code descriptions for any existing codes. Lines workspace field descriptions
Lines workspace field descriptions
Field Claim Type Description ICD International Classification of Diseases (ICD) codes that describe diagnoses. These codes are used for diagnostic, billing, and reporting purposes.
The codes are categorized as
ICD:9orICD:10.- The
ICD:9—code contains three to five characters. The first digit may be alpha or numeric. There is a decimal after the third character with the exception of E codes, which have a decimal after the fourth character. - The
ICD:10—code contains three to seven digits. The first digit is alpha, the second is numeric, and the third through seventh digit are alpha or numeric. A decimal is used after the third character.
Diagnosis Codes Diagnosis codes for the claim. Each diagnosis code has a corresponding diagnosis pointer (with the exception of Institutional)—a single alpha character preceding its corresponding diagnosis code, for example, A: 480.
Note: Diagnosis codes apply to the entire claim line. To associate a Diagnosis code to the Claim Line, enter a value (s) in the Diagnosis Pointer field to point to the Diagnosis code.
- You can enter up to four diagnosis codes for Dental, 12 for Professional, and 26 for Institutional (24 + a principle and admitting diagnosis).
Prin Dx Institutional only Principal Diagnosis code. The original diagnosis code.
Admit Dx Institutional only Admission diagnosis code. The diagnosis code when the patient was admitted.
Line Claim line item identifier.
- Valid claim line numbers are from 1 through the new last claim line number.
Rev Code Institutional only - HIPAA
 HIPAA (Health Insurance Portability and Accountability Act of 1996) is the United States legislation that provides data privacy and security provisions for safeguarding medical information.-compliant, three-digit code consistent with the National Uniform Billing Committee.
HIPAA (Health Insurance Portability and Accountability Act of 1996) is the United States legislation that provides data privacy and security provisions for safeguarding medical information.-compliant, three-digit code consistent with the National Uniform Billing Committee. - Revenue Codes are descriptions and dollar amounts charged for hospital services provided to a patient. The revenue code tells an insurance company whether the procedure was performed in the emergency room, operating room or another department.
-
The claim schedule determines if revenue accounting is necessary for the claim line.
Note: 837I claims, may require Revenue codes.
HCPCS Institutional only The Healthcare Common Procedure Coding System (HCPCS) is a set of codes that standardize identification of medical services, supplies, and equipment.
- There are two sets of codes. The first, or Level I, code set is a five-digit numeric code that contains the Physicians Current Procedural Terminology (CPT) maintained by the American Medical Association.
- The second code set, or Level II is a code set for medical services not included in Level I, such as durable medical equipment, prosthetics, orthotics and supplies. These codes are alpha-numeric and begin with a single letter followed by four numbers.
From Dt Professional and Institutional only Thru Dt Professional and Institutional only End date of service.
Proc Date Dental only Date the procedure was performed—the From date of the service.
PoS Place Of Service. Numeric code describing the location where service was rendered. The codes are defined by the plan administrators but also include basys defaults.
Note: If you change a claim's ToS, you'll be asked if you want to apply the new ToS to all claim lines. ClickYesto update orNoto only change the selected claim line.ToS A code identifying the type of service provided by the service provider. Tooth Number Dental only The tooth number or group of teeth (can include a quadrant of the mouth), the dentist indicated the procedure was performed.
Universal/USA System
1-32—Permanent TeethA-T—Primary TeethUR—Upper Right Quadrant (1-8)UL—Upper Left Quadrant (9-16)LL—Lower Left Quadrant (17-24)LR—Lower Right Quadrant (25-32)- A
+following the tooth number, e.g.A+, means the tooth is supernumerary (an additional tooth beyond the regular number of teeth).
Tooth Surface Dental only Letter codes that identify tooth surfaces.
D—DistalO—OcclusalB—BuccalL—LingualLA—LabialF—FacialI—IncisalG—GroovesM—Mesial
Proc Dental and Professional only Procedure Code—A code that identifies a specific service performed by a service provider.
- Comments associated with the procedure code show above the
Insertbutton.
Dx Ptr Dental and Professional only Diagnosis pointers for the claim line. Diagnosis pointers are a single alpha character preceding its corresponding diagnosis code, for example,
A: 480. They make it easy to refer to and enter a diagnosis code by just using the alpha character.Note: When a claim has only one diagnosis code, the Diagnosis Pointer field for all claim lines will default to A. If there is more than one diagnosis code, the Diagnosis Pointer field will default to blank.
Modifiers Professional and Institutional Procedure code modifiers—office or medical organization-defined codes that provide additional information concerning a particular service and can be used in the service price calculation.
Qty
Quantity. Dollar amount of the service or the number of times the service was provided. The default is 1.
Billed Amt BCode The benefit code representing a benefit or service covered in the Summary Plan Description document (e.g. eye exam, emergency outpatient care or an office medical visit).
See also BCode field behavior and messages.
Svc Prov Professional only Service Provider. ID and Name of the Service Provider.
- This field updates from the header work space, but you can change it.
Hint: If the full name doesn't display, point your mouse at the field to display the full name.
Prepaid If there is a prepaid amount at the claim level (on the Detail viewport), it is automatically distributed to each claim line.
Type—Identifies the source of the prepaid amount, allowed amount, and PPO affiliation:Member,Medicare,Other insurance.Prepaid—The claim amount that was paid previously.Allowed—Applies to Medicare and other insurance. The amount that is allowed for the claim.PPO Flag—Applies to Medicare and other insurance. AYindicates the plan is affiliated with a PPO A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount..
A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount..
Allowed The allowed amount. The considered amount compared to the UCR
 The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. or fee schedule amount and the lesser of the two is the amount allowed for the line item. Columns display calculated amount for each:
The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. or fee schedule amount and the lesser of the two is the amount allowed for the line item. Columns display calculated amount for each:MemberMedicareOther—another insurance provider
Ineligible Code
Code that explains why a claim or portion of a claim isn't eligible for payment. Reasons include duplicate charges, services not covered, and coverage not in effect.
Ineligible Amount Claim or portion of a claim that isn't eligible for payment. The amount that isn't considered for payment.
PPO Flag Preferred Provider Organization (PPO
 A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount.) Flag.
A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount.) Flag.- Click the check box to indicate the insurer provider is affiliated with a PPO.
MedicareOther—another insurance provider
Comments made on the Procedure Code display below the PPO Flag label.
- The
-
Overrides—Allows entry of claim overrides information including Liability, Eligibility, and Stop Loss Payment. Overrides workspace field descriptions
Overrides workspace field descriptions
* indicates a required field
Field Description Claim Overrides Stop Loss Payment
If a benefit payment is too large, it might qualify as a Stop Loss Payment, where the fund office only needs to cover up to a certain amount to avoid using up the fund reserves on one claim.
- Select
YesorNo. The default isNo.
Send LBC Transaction
The Labor BlueCard process enables self-administered benefit funds to access the BlueCross BlueShield (BCBS) provider network to process claims
- If you use the LBC process, but want don't want to send a transaction file to Blue Cross Blue Shield (BCBS) Illinois for a claim, select
No. - If you don't use BCBS as a Trading Partner, the option is disabled.
Liability Patient Liability
Amount the patient owes.
Note: The amount is calculated automatically, but you can override it on the Claim Entry or Processing Overrides workspace.
Provider Liability
Amount that is the provider's responsibility.
-
For example, a provider belongs to a network and bills $90 for a procedure. The network only allows $50. If the claim is paid at 100% (no patient responsibility), then the provider is liable for the remaining $40.
Note: The amount is calculated automatically, but you can override it on the Claim Entry or Processing Overrides workspace.
PPO Discount
The Preferred Provider Organization (PPO
 A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount.) discount is the amount the member saves using a network provider.
A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount.) discount is the amount the member saves using a network provider.- The PPO discount is the difference between the provider's billed amount and the PPO's allowed amount.
- If the plan doesn't use a PPO network, it will be zero.
Note: The amount is calculated automatically, but you can override it on the Claim Entry or Processing Overrides workspace.
FSA Liability Amount that could be FSA
 Accounts offered and administered by employers that provide a way for employees to set aside, out of their paycheck, pretax dollars to pay for the employee’s share of insurance premiums or medical expenses not covered by the employer’s health plan. eligible.
Accounts offered and administered by employers that provide a way for employees to set aside, out of their paycheck, pretax dollars to pay for the employee’s share of insurance premiums or medical expenses not covered by the employer’s health plan. eligible. - Patient Liability—Non-reimbursable Ineligible Amounts.
Note: The amount is calculated automatically, but you can override it on the Claim Entry or Processing Overrides workspace.
Overridden By The operator ID of the person who last entered an override code/amount and the time. Eligibility Subgroup *
Code and name of the active subgroup
 A way to categorize group members into a certain set for benefit plans (e.g. active and retired employees). Subgroup distinctions are only used in Claims, COBRA and Eligibility. that is associated with a current health plan.
A way to categorize group members into a certain set for benefit plans (e.g. active and retired employees). Subgroup distinctions are only used in Claims, COBRA and Eligibility. that is associated with a current health plan. - Only active subgroups display in the list.
- If there's no active eligibility for a patient, the Eligibility override fields default (Subgroup, Plan, Coverage) to the patient's last active eligibility.
Plan * Code and name of the benefit plan
 A benefit plan identifies the benefits an individual receives as the result of his or her association with a subgroup. associated with the selected subgroup.
A benefit plan identifies the benefits an individual receives as the result of his or her association with a subgroup. associated with the selected subgroup. - If there's no active eligibility for a patient the Eligibility override fields default (Subgroup, Plan, Coverage) to the patient's last active eligibility.
Coverage * The coverage code identifies who is covered by a benefit plan type, for example, individual or family.
- Choices are limited to coverage options that apply to the selected benefit plan and the patient's relationship to the member.
Pay Option that allows you to pay an ineligible claim if you have the appropriate permissions.
Ineligible Option that allows you to designate a paid claim as ineligible. Overridden By The operator ID of the person who last entered an eligibility override code/amount and the time. PPO PPO Preferred Provider Organization (PPO
 A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount.). Code and PPO name.
A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount.). Code and PPO name. - Choices are limited to PPOs for the selected benefit Plan and claim dates.
-
If there's more than one line in the claim, once you choose the PPO, an Override PPO window displays:
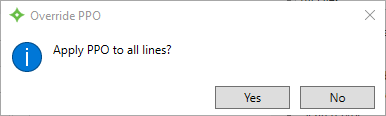
Click
Yesto apply the override to all the claim's lines, or clickNoto only apply to the selected line.
Overridden By The operator ID of the person who last entered a PPO override code/amount and the time. Procedure (applies to Institutional claims) Procedure If both Revenue and HCPCS codes are present on a claim line, the override feature becomes enabled so you can choose which codes determine the claim eligibility and pricing.
Overridden By The operator ID of the person who last entered a Procedure override code/amount and the time. - Select
-
Links—Allows you to select disputes associated with claims including the original and adjusted claim numbers and linked illnesses and admissions. Links workspace field descriptions
Links workspace field descriptions
Field Description Lists any disputes associated with the patient in the following format:
- Dispute Type; Status; Date it was opened; Recovered Amount; Operator; Comment. For example,
AUTO; C; 1/2/2014; 7/20/2015; 12.00; USERID
Adjusted To Claim
Reference number of the new claim that was adjusted from the original claim.
(Adjusted To Claim) Overridden by
Operator ID who entered the Adjusted To Claim override information.
Adjusted From Claim
Reference number of the original claim that was adjusted to a new claim.
Note: You must be authorized to enter Adjusted From Claim information.
- If there is a value in Adjusted From Claim but no operator override information shows below it, this means the adjustment was system- generated and you can't change it.
(Adjusted From Claim) Overridden by ID of the operator who entered the Adjusted From Claim override information.
Linked Illness for Line Lists admissions associated with the patient in the following format:
- Diagnosis code; Description; Incurred Date; Operator. For example
301.2; SCHIZOID PERSONALITY ; 2/2/2014; RYANM.
See also Linked illnesses messages.
Linked Admission for Line Lists admissions associated with the patient in the following format:
- Admission Date; Discharge Date; #Used of #Approved; Operator; Comment. For example,
1/3/2014; 12/13/2014; 1 of 1; RYANM
See also Linked admissions messages
- Dispute Type; Status; Date it was opened; Recovered Amount; Operator; Comment. For example,
-
Duplicates—Displays information when a claim line is similar enough to other claims on the system and could be a duplicate. Possible matches show to validate or determine if there is a duplicate submission. When aP25-Pended for Duplicatecode displays after validating a possible duplicate claim, you're guided to the Institutional Claim Duplicates workspace. Duplicates workspace field descriptions
Duplicates workspace field descriptions
Column Description Ref No.
Claim reference number.
Line No.
The claim line number. If the entire claim is in Held or Audit status, then this field is blank.
Status
The status of the claim. See Claim statuses for descriptions.
SvcProvider
The provider who renders the services submitted by the billing provider.
From Dt
Start date of procedure/service for the claim line item.
Thru Dt
End date of procedure/service for the claim line item. Billed Amt
The amount billed to the member.
Considered Amt
The amount considered for payment. It is calculated as follows: Billed Amount - Ineligible Amount.
Net Covered Amt
The amount that is covered under the plan rules. It is calculated as follows: Covered Amount - COB adjustments.
Paid Amt
The actual benefit amount paid. It is calculated as follows: Net Covered Amount - Discount Amount.
Procedure
A code that identifies a specific service performed by a service provider.
Diag
International Classification of Diseases (ICD) codes that describe diagnoses. These codes are used for diagnostic, billing, and reporting purposes.
The codes are categorized as
ICD:9orICD:10.- The
ICD:9—code contains three to five characters. The first digit may be alpha or numeric. There is a decimal after the third character with the exception of E codes, which have a decimal after the fourth character. - The
ICD:10—code contains three to seven digits. The first digit is alpha, the second is numeric, and the third through seventh digit are alpha or numeric. A decimal is used after the third character.
TOS
A code identifying the type of service provided by the service provider.
POS
Place Of Service. Numeric code describing the location where service was rendered. The codes are defined by the plan administrators but also include basys defaults.
BCode The benefit code representing a benefit or service covered in the Summary Plan Description document (e.g. eye exam, emergency outpatient care or an office medical visit). Illness Amount applied to an illness limitation (deductible, count of days, etc.)
Admission Date of admission for the line item illness.
Bill Prov The individual or organization that issued the bill for the services listed on the claim.
Tooth The tooth number or group of teeth (can include a quadrant of the mouth), the dentist indicated the procedure was performed.
Universal/USA System
1-32—Permanent TeethA-T—Primary TeethUR—Upper Right Quadrant (1-8)UL—Upper Left Quadrant (9-16)LL—Lower Left Quadrant (17-24)LR—Lower Right Quadrant (25-32)- A
+following the tooth number, e.g.A+, means the tooth is supernumerary (an additional tooth beyond the regular number of teeth).
International/FDI System
- valid teeth:
- 11–18, 21–28, 31–38, 41–48, 51–55, 61–65, 71–75, 81–85, and 99
- valid quadrants:
- 10=11–18, 20=21–28, 30=31–38, 40=41–48
- valid sextants:
- 04=11–13, 21–23, 05=24–28, 06=34–38, 07=31–33, 41–43, 08=44–48
Surface Letter codes that identify tooth surfaces.
D—DistalO—OcclusalB—BuccalL—LingualLA—LabialF—FacialI—IncisalG—GroovesM—Mesial
Bill Type Bill type is a 4-digit code that applies to institutional claims, where each digit identifies specific information:
- 1st digit is a leading zero and isn't used in Service.
- 2nd digit is the facility type.
- 3rd is the bill classification.
- 4th is the submission frequency.
Operator Operator who entered the duplicate claim information. HCPCS The associated alpha-numeric HCPCS  HCFA Common Procedure Coding System (HCPCS) Procedure Code for institutional (hospital) claims. code.
HCFA Common Procedure Coding System (HCPCS) Procedure Code for institutional (hospital) claims. code.Revenue Code The associated numeric revenue code  Revenue codes are three-digit codes that affect reimbursement and represent the healthcare services provided for a payer..
Revenue codes are three-digit codes that affect reimbursement and represent the healthcare services provided for a payer.. - The
-
Calc Detail—Shows how the amount covered by the fund is calculated for the selected claim line (the amounts applied to deductibles, the coinsurance percentage used, etc.). With the appropriate permissions and settings, these values can be changed here. Calc Detail workspace field descriptions
Calc Detail workspace field descriptions
* indicates a required field
Column Description Pay Type *
A code that indicates the payment type.
A—Alternative PaymentAR#—Alternative RevertedB—BasicBR#—Basic RevertedM—Major Medical Usually means that benefits are paid subject to deductibles and co-insurance, leaving the claimant with an out-of-pocket balance.
Usually means that benefits are paid subject to deductibles and co-insurance, leaving the claimant with an out-of-pocket balance.MR#—Major Medical RevertedS—Split Payment
Allowed *
The allowed amount. The considered amount compared to the UCR
 The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. or fee schedule amount and the lesser of the two is the amount allowed for the line item.
The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. or fee schedule amount and the lesser of the two is the amount allowed for the line item. Annual
Amount applied to an annual deductible.
Lifetime
Amount applied to a lifetime deductible.
Copay
Amount applied to a copay deductible.
Illness
Amount applied to an illness deductible.
Day
Amount applied to a daily deductible.
Month
Amount applied to a monthly deductible.
Other
Deductible amount that doesn't fall into one of the other deductible categories.
Pat Cov The patient covered amount under the No Surprises Act (NSA). The amount covered by providers. It is calculated as follows: (Allowed Amount - Deductibles) multiplied by (Co-Insurance %). Cov Adj The coverage adjustment amount under the No Surprises Act (NSA). It's the NSA covered amount based on the out-of-network QPA amount less than the member liability.
Co-Insurance %
The percentage of the benefit that is the claimant's responsibility after the claimant has met deductible amounts.
Covered
The patient covered amount minus the covered adjustment amount.
COB
The Coordination of Benefit (COB) adjustment amount. This is any amount that has been paid by other insurance or is being drawn from coverage savings.
Net
The amount that is covered under the plan rules. It is calculated as follows: Covered Amount - COB adjustments.
-
Cap Detail—Shows how the system determined the pricing for the claim line and calculated the allowed amount. Cap Detail workspace field descriptions
Cap Detail workspace field descriptions
Field Description Header Fund Code that identifies the fund associated with the claim. A fund is a legal entity for the distributions of money.
Group Group associated with the claim. A group refers to a set of members with similar characteristics, for example, the same type of work or geographic location.
Subgroup The active subgroup
 A way to categorize group members into a certain set for benefit plans (e.g. active and retired employees). Subgroup distinctions are only used in Claims, COBRA and Eligibility. that is associated with a current health plan.
A way to categorize group members into a certain set for benefit plans (e.g. active and retired employees). Subgroup distinctions are only used in Claims, COBRA and Eligibility. that is associated with a current health plan. Benefit Plan Benefit plan under which the claim was processed. PPO A code that represents the provider's PPO  A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount. affiliation.
A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount. affiliation.Coverage The coverage code identifies who is covered by a benefit plan type, for example, individual or family. Schedule Code defined by the plan administrators that identifies the claim schedule  Defines parameters for Apps, contracts, status', pay, benefits, rules, etc...
Defines parameters for Apps, contracts, status', pay, benefits, rules, etc...Schedule Detail Reference number that identifies the parameters used to process the claim line. Table Pay Type A code that indicates the payment type.
A—Alternative PaymentAR#—Alternative RevertedB—BasicBR#—Basic RevertedM—Major Medical Usually means that benefits are paid subject to deductibles and co-insurance, leaving the claimant with an out-of-pocket balance.
Usually means that benefits are paid subject to deductibles and co-insurance, leaving the claimant with an out-of-pocket balance.MR#—Major Medical RevertedS—Split Payment
Cap Code The Cap Code
 A code setup within the schedule to identify the source of the pricing information. used to determine how the allowed amount is calculated.See Cap Codes and descriptions for details.
A code setup within the schedule to identify the source of the pricing information. used to determine how the allowed amount is calculated.See Cap Codes and descriptions for details.Path The path
 The pricing methods used and the order, established in the schedule. code used to determine the UCR
The pricing methods used and the order, established in the schedule. code used to determine the UCR The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. pricing information. See Path codes and descriptions. The value of the Procedure source code is displayed with the Path, if data exists.
The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. pricing information. See Path codes and descriptions. The value of the Procedure source code is displayed with the Path, if data exists.Cap Amount Amount based on the selected path.
Percentage Percentage of the cap amount that was allowed. Adjustment Amount by which the cap amount was adjusted. Adj Code A code that identifies the adjustment reason.
A—Already Allowed (under a prior pay type)C—Over ConsideredM—MaximumO—Operator OverrideR—Reversion
Dev Type The deviation type applied to the UCR.
A—Threshold Amount. Increases the UCR by a dollar amount if the considered amount exceeds the UCR.F—Flat Fee. Allows the UCR The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. if it is within a dollar amount of the considered amount.
The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. if it is within a dollar amount of the considered amount. S—Threshold Percent. Increases the UCR by a percentage amount if the considered amount exceeds the UCR.P—Percentage. Allows the UCR if it is within a specified percentage of the considered amount.
Dev Amount Deviate Amount. Amount or percentage used as a result of the deviate type applied. Allowed The allowed amount. The considered amount compared to the UCR
 The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. or fee schedule amount and the lesser of the two is the amount allowed for the line item.
The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. or fee schedule amount and the lesser of the two is the amount allowed for the line item. Original Quantity Original billed quantity when a quantity maximum has been hit. Below table Zip Service provider's zip code used in determining pricing for a geographic area. GEO Used The geographical code (or Zip prefix) used in determining pricing for a geographical area.
Region Used Region code associated with the procedure source to further define pricing.
QPA Amount The qualifying payment amount. Generally, the median of contracted rates for a specific service in the same geographic region within the same insurance market as of January 31st, 2019. OON Amount The out-of-network allowed amount. -
Summary—Displays a payment summary of the claim lines. Summary workspace field descriptions
Summary workspace field descriptions
Column Description #
Billed
The amount billed for the claim.
Considered
The amount considered for payment. It is calculated as follows: Billed Amount - Ineligible Amount.
Allowed
The allowed amount. The considered amount compared to the UCR
 The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. or fee schedule amount and the lesser of the two is the amount allowed for the line item.
The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. or fee schedule amount and the lesser of the two is the amount allowed for the line item. Covered
The amount covered by providers. It is calculated as follows: (Allowed Amount - Deductibles) multiplied by (Co-Insurance %).
Net Covered
The amount that is covered under the plan rules. It is calculated as follows: Covered Amount - COB adjustments.
Discount
This discount amount. The discount is either:
- Net Covered Amount multiplied by Discount Percentage
OR
- a configurable discount amount ( e.g. a provider discount or a claim schedule discount)
MS Discount
The member share discount. This is calculated as follows: Discount (previous column) - a Discount Amount.
Disc Code
Discount Code. Code that identifies and defines the discount taken on the net covered amount.
Note: Discounts taken on billed or considered amounts are considered as ineligible amounts.
The actual benefit amount paid. It is calculated as follows: Net Covered Amount - Discount Amount.
-
Prepricing—Medicare or other prepaid amounts, allowed amount, ineligible code and amount, considered amount, and the claim invoice number. Prepricing workspace field descriptions
Prepricing workspace field descriptions
Column Description Click to display or enter prepaid codes and amounts for Medicare or Other providers.
The claim line number.
Amount of the claim that was prepaid.
Allowed Amt
The allowed amount. The considered amount compared to the UCR
 The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. or fee schedule amount and the lesser of the two is the amount allowed for the line item.
The Usual, Customary, and Reasonable amounts allowed for a procedure. UCR compares the charge for a procedure to the amount other doctors have charged for the procedure. UCR data can be external data obtained from HIAA or MDR by geographic area, or can be compiled internally. The allowed determination can be based on a percentile; for example, the 85th percentile would cover the charges of 85% of the doctors who submitted bills. or fee schedule amount and the lesser of the two is the amount allowed for the line item. Inelg Code
Charges might not be eligible for payment for many reasons including duplicate charges, services not covered, and coverage not in effect.
Code—A code and description that explains why a claim amount was denied.Amount—The claim amount that is ineligible.
Considered Amt
The amount considered for payment. It is calculated as follows: Billed Amount - Ineligible Amount.
Ineligible Amt
Charges might not be eligible for payment for many reasons including duplicate charges, services not covered, and coverage not in effect.
Code—A code and description that explains why a claim amount was denied.Amount—The claim amount that is ineligible.
Invoice#
Invoice number for the claim.
-
Messages—Shows the claim and line comments that will display on the member or provider Explanation of Benefits (EOB EOBs are sent to members and payees to inform them of the disposition of claims. Typically an EOB identifies the date and type of service, the billed amount, deductibles, co-insurance, and an explanation of any ineligible charges. An EOB can also be a helpful tool in identifying fraudulent claims, as the member receives notification even when payment is made to the provider. An EOB isn't a bill.).
EOBs are sent to members and payees to inform them of the disposition of claims. Typically an EOB identifies the date and type of service, the billed amount, deductibles, co-insurance, and an explanation of any ineligible charges. An EOB can also be a helpful tool in identifying fraudulent claims, as the member receives notification even when payment is made to the provider. An EOB isn't a bill.).  Messages workspace table field descriptions
Messages workspace table field descriptions
Accumulators—Displays the accumulators and accumulator descriptions associated with the claim line.
The navigator shows you two key editing validation messages at the bottom of the Claims Entry or Processing tabs.
You'll find the validation messages at the bottom of the Claims tab, the upper-right of the Claims Entry, or the bottom lower-right of the Star menu.
- The first key item to note are any edits that have to be resolved for the claim.
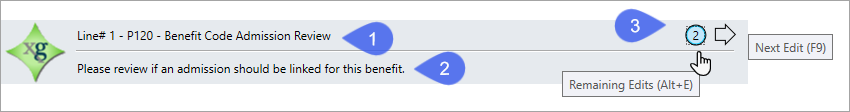
- Instructions on how to resolve the edit display in the second area, below the edit.
- The next area is sometimes referred to as the 'edits rotator'. Any remaining edits show here.
- Click the circle to show the edits window or use
Alt+E.
- Click the arrow to advance through the edit or use
F9. See Guided Processing System (GPS) for additional information.
- Click the circle to show the edits window or use
When you click ![]() at the left bottom of a Claims processing or entry tab, the star menu displays.
at the left bottom of a Claims processing or entry tab, the star menu displays.
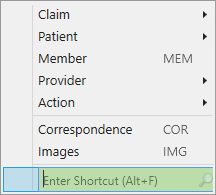
See Star menu for more information.